What if your family’s diabetes didn’t start in your kitchen? What if it started 150 years ago during a famine?
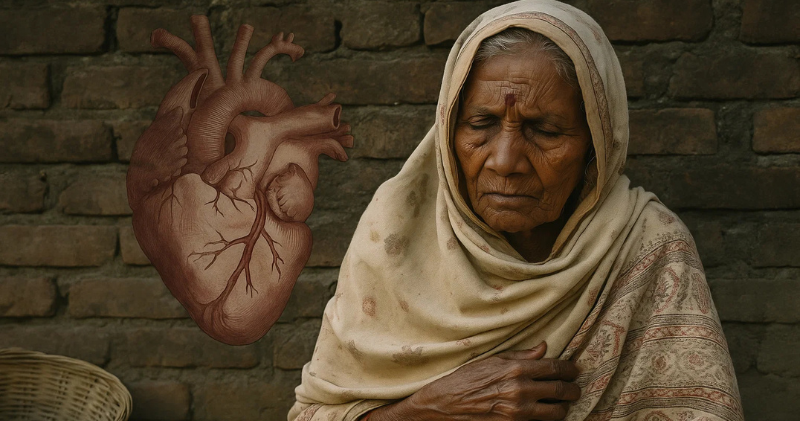
Here’s a shocking question: Why do so many South Asian families have the same health problems? Diabetes at 45. Heart attacks at 50. High cholesterol despite eating home-cooked food.
We often blame our genes or our modern lifestyle. But new science suggests something much deeper is happening. The famines that killed millions of our ancestors may have changed our bodies forever. And those changes are still affecting us today.
This isn’t about blaming anyone. It’s about understanding why South Asians get sick differently than other people. And more importantly, what we can do about it.
The Famines That Changed Everything
Let’s start with some hard facts about what happened during British rule in India.
Before the British: In 2,000 years before British rule, India had about 17 major famines. That’s roughly one every 100+ years.
During British rule (1757-1947): India had an estimated 31 major famines in just 190 years. That’s one every 6 years.
This wasn’t bad luck. This was the result of policies that put British profits over Indian lives.
The Big Three Famines
1770 – The Great Bengal Famine
- Killed 10 million people (1/3 of Bengal’s population)
- The British East India Company kept collecting taxes even as people starved
- They exported grain to England while Indians died
1876-1878 – The Great Famine of South India
- Killed 5.5 million people
- Covered an area the size of France
- British officials refused to stop grain exports during the worst months
1943 – The Bengal Famine
- Killed 3 million people during World War II
- When officials told Winston Churchill about the deaths, he reportedly asked “Why hasn’t Gandhi died yet?”
How the British Created Famines
The British didn’t just ignore famines. They created conditions that made them worse:
Cash crops over food: They forced farmers to grow cotton and indigo instead of rice and wheat. This made money for Britain but left people unable to feed themselves.
Free trade during starvation: Even during famines, the British kept exporting grain from India to global markets.
Tax collection during disasters: When crops failed, the British still demanded tax payments. Farmers had to sell their seed grain just to pay taxes.
Cheap relief: When they provided famine relief, it was intentionally kept minimal to save money.
As one economist put it: these famines weren’t about lack of food. They were about lack of access to food.
What Famines Do to Bodies (And Genes)
When people face starvation repeatedly, their bodies learn to survive. But those survival changes can hurt health later.
The “Thrifty Gene” Theory
In 1962, scientist James Neel came up with an idea called the “thrifty gene hypothesis.” Here’s what it means:
During famines: Bodies that could store fat efficiently and survive on very little food had a better chance of living through starvation.
After famines: Those same bodies kept the survival programming. They continued storing fat efficiently and being very careful with energy.
In modern times: Bodies still programmed for famine now face constant food availability. The result? Weight gain, diabetes, and heart disease.
How This Affects Genes
Scientists have discovered something amazing: trauma can change how genes work without changing the genes themselves. This is called “epigenetics.”
Example 1 – Dutch Hunger Winter: During World War II, western Netherlands faced severe famine. Babies born during this time had normal birth weights. But 60 years later, they had higher rates of diabetes and heart disease. Their genes had been “programmed” by famine exposure.
Example 2 – Chinese Famine: People born during China’s famine of 1959-1961 had higher cholesterol and more diabetes as adults. Even their children (who never experienced famine) had higher diabetes rates.
The South Asian Connection: South Asians experienced far more frequent and severe famines than these populations. The genetic programming may be even stronger in our community.
Why South Asians Get Sick Differently
Today, South Asians face unique health challenges that may trace back to this famine history:
The Numbers Don’t Lie
- Heart disease: South Asians get heart attacks 5-10 years earlier than other groups
- Diabetes: We’re up to 6 times more likely to develop diabetes than white people
- Weight: We develop diabetes at much lower weights (BMI 22-23 vs 28-30 for others)
The “Skinny Fat” Problem
Many South Asians look thin but have dangerous fat around their organs. Doctors call this “TOFI” – Thin Outside, Fat Inside. This reflects bodies that store fat internally where it causes metabolic problems but isn’t visible.
Strange Blood Test Results
South Asians often have:
- High triglycerides (blood fats) despite vegetarian diets
- Low HDL (good cholesterol)
- High Lp(a) – a genetic cholesterol factor affecting 30% of South Asians
- Small, dense LDL particles – the dangerous type of cholesterol
Early Disease, Normal Weight
While other populations get diabetes when overweight, South Asians can become diabetic at normal weights. This “skinny diabetic” pattern may reflect famine-adapted bodies.
The Science Behind Inherited Trauma

This isn’t just theory. Multiple studies prove that famine effects can pass to future generations:
Dutch Studies
Researchers studied people whose mothers were pregnant during the 1944-45 Dutch famine. 60 years later, these people had:
- Different patterns of gene activity
- Higher diabetes rates
- More heart disease
- Changes in genes controlling metabolism
Chinese Studies
People born during China’s 1959-1961 famine showed:
- Higher cholesterol as adults
- More diabetes
- Metabolic problems that appeared in their children too
Animal Studies
Research in animals confirms that starvation changes can pass to offspring through:
- Changes in gene activity (not gene structure)
- Stress hormone programming
- Metabolic efficiency programming
What You Can Do Right Now
Understanding this history isn’t about dwelling on the past. It’s about protecting your future. When you know your body may carry “famine genes,” you can take smart action.
Get the Right Tests Early
Don’t wait until your 40s or 50s. Ask your doctor for these tests in your 20s and 30s:
HbA1c: Shows your average blood sugar over 3 months. Should be under 5.7%.
ApoB: Counts dangerous cholesterol particles. More accurate than regular cholesterol tests for South Asians.
Lp(a): A genetic cholesterol factor. If high, you need extra heart protection.
Triglycerides: Should be under 100, not the “normal” 150.
Waist-to-hip ratio: Better than BMI for detecting dangerous belly fat.
Eat Like Your Genes Expect
Your body evolved for feast-and-famine cycles. Work with that reality:
Time your eating: Give your body breaks between meals, like natural fasting periods.
Choose whole foods: Eat foods your great-grandparents would recognize.
Control portions: Remember that traditional serving sizes were much smaller.
Add protein to every meal: This helps control the blood sugar spikes your body is prone to.
Fill up on fiber: Vegetables, lentils, and whole grains slow down sugar absorption.
Move After Meals
This one habit can change everything. A 10-15 minute walk after eating can:
- Reduce blood sugar spikes by 30-50%
- Improve insulin sensitivity
- Signal your genes that energy is being used, not stored
Manage Stress Like Medicine
Chronic stress triggers the same biological responses as famine. Your body thinks it’s starving when you’re stressed. So stress management isn’t luxury – it’s medical necessity:
- Sleep 7-8 hours: Essential for metabolic health
- Practice relaxation: Meditation, deep breathing, or yoga
- Stay connected: Social isolation increases stress hormones
- Get help: Don’t hesitate to talk to counselors about stress
Know Your Family History
Document patterns of diabetes, heart disease, and early death in your family. Share this information with:
- Your doctor (helps assess your risk)
- Your family members (motivates them to get tested)
- Your children (helps them understand their risks)
Breaking the Cycle
The famines ended in 1947, but their biological effects don’t have to define your future.
Your ancestors survived incredible hardship. The same genes that helped them survive famines can help you thrive today – if you understand how to work with your biology.
This knowledge is power. When you know why South Asians get sick differently, you can:
- Get tested earlier
- Eat more strategically
- Exercise more effectively
- Manage stress better
You’re not doomed by your genes. You’re informed by them. And information leads to better choices.
Your family’s future depends on what you do today. The next generation doesn’t have to repeat the same health patterns. Start the conversation. Share this knowledge. Break the cycle.
The British may have left India 80 years ago, but the biological damage they caused lives on in our cells. However, understanding that damage is the first step to healing it.
Your great-grandparents endured famines so you could exist. Honor their survival by taking care of the body they passed down to you.
Take Action Today
Step 1: Take our South Asian Heart Risk Quiz to see how famine history might affect your health
Step 2: Download our “Break the Cycle” action guide with specific steps for your age group
Step 3: Share this article in your family WhatsApp group. Start the conversation about early testing and prevention
Remember: You can’t change your history, but you can change your future. Start today.
Sources:
Timeline of famines in British India: https://en.wikipedia.org/wiki/Timeline_of_major_famines_in_India_during_British_rule
British colonial mortality research: https://www.aljazeera.com/opinions/2022/12/2/how-british-colonial-policy-killed-100-million-indians
Dutch Hunger Winter studies: https://pmc.ncbi.nlm.nih.gov/articles/PMC2579375/
Chinese famine epigenetics: https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-019-0676-3
South Asian diabetes risk: https://medcraveonline.com/JDMDC/increased-prevalence-of-type-2-diabetes-in-south-asian-population-ndash-a-genetic-perspective.html