Ravi got the news at 45. His coronary calcium scan showed significant plaque buildup. The doctor explained that his arteries were like old pipes—clogged with deposits that had been building for years.
“Is this permanent?” Ravi asked. “Will it just keep getting worse?”
His cardiologist paused. “Most doctors used to think plaque only gets worse. But new research shows something amazing. With the right approach, you can actually shrink plaque. It’s not easy, but it’s possible.”
Six months later, Ravi’s follow-up tests showed something remarkable. His plaque had started to stabilize. Some areas had even shrunk slightly.
How did he do it? And more importantly, can you do it too?
What Is Plaque? Why Does It Matter?
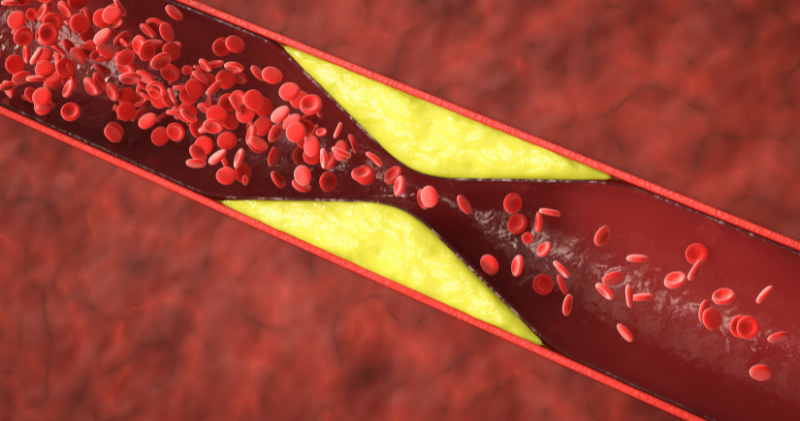
Arterial plaque is like rust in your body’s highways. It’s made of cholesterol, fat, calcium, and other substances that
stick to artery walls over time.
How plaque forms:
- LDL (“bad”) cholesterol gets into artery walls
- Your immune system tries to clean it up
- This creates inflammation
- More cholesterol and inflammatory cells pile up
- The deposit grows larger and harder over time
Two types of plaque: Stable plaque: Hard and calcified. Less likely to break off suddenly. Still narrows arteries and reduces blood flow.
Unstable plaque: Soft with a thin cap. More dangerous because it can rupture suddenly. When unstable plaque breaks, it forms blood clots that cause heart attacks.
Why plaque matters: Even small amounts of plaque increase heart attack risk. Plaque doesn’t just block arteries like a clogged drain. It makes arteries stiff and prone to dangerous ruptures.
South Asian connection: We develop plaque earlier and in different patterns than other groups. We’re more likely to have plaque in multiple arteries, even when young.
The key question: once you have plaque, are you stuck with it forever?
Can It Be Reversed? Yes… But Slowly
The answer surprised researchers for decades. For years, doctors thought plaque only got worse. New studies show plaque can actually shrink and become more stable.
What the research shows: Famous studies like the Lyon Diet Heart Study and Dr. Dean Ornish’s research proved plaque reversal is possible. People who made dramatic lifestyle changes saw their plaque shrink by 5-10% over 1-2 years.
Recent breakthrough studies:
- PCSK9 inhibitor drugs can shrink plaque by 1-2% per year
- Intensive statin therapy reduces plaque volume
- Plant-based diets combined with exercise show plaque regression
- Even partial improvements reduce heart attack risk significantly
What “reversal” really means: Plaque reversal doesn’t mean arteries go back to being like new. Instead, dangerous unstable plaque becomes more stable. Some plaque shrinks. New plaque formation stops.
The reality check: Reversal requires major changes. Half-hearted efforts won’t work. You need intensive lifestyle changes plus often medications.
Why this matters for South Asians: Since we develop plaque younger, we have more time to benefit from reversal strategies. Starting aggressive treatment in your 40s or 50s can prevent heart attacks in your 60s and 70s.
But reversal isn’t quick or easy. It requires commitment and usually medical supervision.
Diet, Exercise, and Medications
Plaque reversal needs a three-part approach. Diet alone isn’t enough. Exercise alone isn’t sufficient. You need all three working together.
Diet Changes That Work: Mediterranean Diet: Proven to reverse plaque in studies. Focus on olive oil, fish, vegetables, fruits, nuts, and whole grains. Limit red meat and processed foods.
Plant-Forward Diet: Dr. Ornish’s research used very low-fat, mostly plant-based diets. Participants ate less than 10% of calories from fat. This is extreme but effective.
Key dietary principles:
- Reduce saturated fat to less than 7% of calories
- Eliminate trans fats completely
- Eat 5-9 servings of fruits and vegetables daily
- Choose whole grains over refined grains
- Limit sugar and processed foods
Exercise Requirements: Moderate exercise isn’t enough for plaque reversal. You need more intensive activity:
- 45-60 minutes of aerobic exercise, 5-6 days per week
- Include both moderate and vigorous intensity
- Add strength training 2-3 times per week
- Aim for 300+ minutes of exercise weekly
Medications That Help: Statins: The most proven medications for plaque reversal. High-intensity statins (like atorvastatin 80mg) can shrink plaque and make it more stable.
PCSK9 Inhibitors: Newer, expensive drugs that dramatically lower LDL cholesterol. Studies show they can reverse plaque when combined with statins.
Blood Pressure Medications: ACE inhibitors and ARBs don’t just lower blood pressure. They also stabilize plaque and reduce inflammation.
Promising Natural Options: Nattokinase: This enzyme from fermented soybeans shows exciting results. A study of 76 patients found that nattokinase (6,000 FU daily) significantly reduced plaque size and artery thickness over 26 weeks. Another large study with 1,062 participants showed that higher doses (10,800 FU daily) reduced plaque by 66-95% over 12 months.
Vitamin K2 (MK-7): This vitamin helps keep calcium in bones and out of arteries. Some studies show it can slow calcium buildup in arteries. However, results are mixed. While it may help prevent new calcium deposits, reversing existing calcification is more challenging.
Important note: These natural supplements show promise but need more research. Always discuss with your doctor before adding them, especially if you take blood thinners.
Realistic Timelines for Change
Managing expectations is crucial. Plaque reversal happens slowly.
What happens when:
First 3 months: Plaque stabilization begins. Unstable plaque develops thicker, stronger caps. Less likely to rupture suddenly.
6-12 months: Some soft plaque begins to shrink. Blood flow may improve slightly. Inflammatory markers in blood decrease.
1-2 years: Measurable plaque regression shows up on scans. Studies show 5-10% reduction in plaque volume with intensive treatment.
2-5 years: Continued slow improvement. Heart attack risk continues to decrease. Some people see dramatic improvements.
Important notes:
- Not everyone responds the same way
- Genetic factors affect how much reversal is possible
- Age matters—younger people often see better results
- Compliance is everything—missing medications or diet breaks slow progress
Realistic expectations:
- Don’t expect normal arteries after treatment
- Small improvements make big differences in heart attack risk
- Even stopping progression is a major victory
- Focus on long-term heart health, not perfect test results
South Asian considerations: We may need more aggressive treatment to see the same results as other groups. Our genetic predisposition means we often need both lifestyle changes AND medications.
Did You Know? Plaque can shrink—but only with serious lifestyle changes and, often, medications. Studies show that intensive treatment combining very low-fat diets, regular exercise, and high-dose statins can reduce plaque by 5-10% over 1-2 years. Even small reductions dramatically lower heart attack risk.
When to Seek Medical Help
Not everyone needs aggressive plaque reversal treatment. But some people should pursue it actively.
You should consider intensive plaque reversal if you have:
- Coronary calcium score over 100
- Known coronary artery disease
- Previous heart attack or stent placement
- Strong family history of early heart disease
- Multiple risk factors (diabetes, high blood pressure, high cholesterol)
Tests that help guide treatment: Coronary Calcium Scan: Shows how much plaque you have. Scores over 100 suggest significant plaque burden.
Coronary CT Angiogram: More detailed test that shows plaque location and type. Can distinguish stable from unstable plaque.
Carotid Ultrasound: Checks for plaque in neck arteries. Often mirrors what’s happening in heart arteries.
Advanced Blood Tests: ApoB, Lp(a), and inflammatory markers help assess risk and monitor treatment response.
Working with specialists: Preventive Cardiologist: Specializes in preventing heart disease progression.
Best choice for plaque reversal programs.
Lipidologist: Expert in cholesterol and lipid disorders. Helpful for complex cases requiring multiple medications.
What to expect from treatment:
- Frequent monitoring with blood tests
- Possible side effects from intensive medications
- Need for lifestyle coaching or counseling
- Regular follow-up scans to track progress
Red flags that need immediate attention:
- New chest pain or pressure
- Shortness of breath with mild activity
- Unusual fatigue or weakness
- Family member has sudden heart attack
Action Steps
Start your plaque reversal journey with these concrete steps:
Try the Mediterranean or plant-forward diet: Start this week by adding olive oil, fish twice weekly, and extra vegetables to every meal. Reduce red meat to once per week. Cut out processed foods and sugary drinks. Consider working with a nutritionist who understands plaque reversal diets.
Quit smoking now: Smoking accelerates plaque formation and prevents reversal. Every cigarette damages arteries further. Use nicotine replacement, prescription medications, or smoking cessation programs. Ask your doctor about varenicline or bupropion to help with cravings.
Ask about statins if you have plaque: If your coronary calcium score is over 100 or you have known plaque, discuss high-intensity statin therapy with your doctor. Don’t worry about mild side effects—the heart attack prevention benefits far outweigh risks for most people.
Consider nattokinase supplementation: Ask your doctor about nattokinase (6,000-10,800 FU daily) if you have plaque buildup. Research shows it can reduce plaque size and improve artery flexibility. Make sure your doctor knows all supplements you take, especially if you’re on blood thinners.
Add vitamin K2 (MK-7) if appropriate: Consider 90-180 mcg daily of vitamin K2 MK-7 to help prevent calcium deposits in arteries. This works best for prevention rather than reversing existing calcification. Avoid if you take warfarin or similar blood thinners.
Increase exercise intensity gradually: Work up to 45-60 minutes of exercise most days. Start where you are now and add 5-10 minutes weekly. Include both cardio and strength training. Consider working with a trainer who understands cardiac rehabilitation.
Frequently Asked Questions
Q: Can I reverse plaque with diet and exercise alone, without medications? A: Some people can, but it’s difficult and usually requires very strict plant-based diets with less than 10% fat. Most people need medications like statins to achieve meaningful plaque reversal. Natural supplements like nattokinase may help, but shouldn’t replace proven treatments when needed.
Q: Is it worth trying to reverse plaque if I’m over 60? A: Absolutely. Studies show benefits at any age. Even if you can’t fully reverse plaque, stabilizing it and preventing new plaque formation significantly reduces heart attack risk. It’s never too late to start.
Q: I’ve heard about nattokinase and vitamin K2. Can these natural supplements help reverse plaque? A: Research shows nattokinase (6,000-10,800 FU daily) can significantly reduce plaque size and artery thickness. Vitamin K2 MK-7 may help prevent new calcium deposits in arteries, but results for reversing existing calcification are mixed. These supplements show promise but need more research. Always discuss with your doctor, especially if you take blood thinners.
References
- Ornish, D., et al. (1998). Intensive lifestyle changes for reversal of coronary heart disease. JAMA, 280(23), 2001-2007.
- Nicholls, S.J., et al. (2011). Effect of two intensive statin regimens on progression of coronary disease. New England Journal of Medicine, 365(22), 2078-2087.
- Chen, H., et al. (2022). Effective management of atherosclerosis progress and hyperlipidemia with nattokinase: A clinical study with 1,062 participants. Frontiers in Cardiovascular Medicine, 9, 964977.
- Kim, J.Y., et al. (2017). A clinical study on the effect of nattokinase on carotid artery atherosclerosis and hyperlipidaemia. Chinese Journal of Integrative Medicine, 24(4), 245-252.
- Knapen, M.H., et al. (2015). Menaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women. Thrombosis and Haemostasis, 113(5), 1135-1144.
- Kurnatowska, I., et al. (2015). Effect of Vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3-5. Polish Archives of Internal Medicine, 125(9), 631-640.
- Goff, D.C., et al. (2014). 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Circulation, 129(25), S49-S73.
If this helped you, please share it with someone you love.